Clinical and histologic evaluation of a fractional radiofrequency treatment of wrinkles and skin texture with novel 1‐mm long ultra‐thin electrode pins
Abstract
Background: Fractional radiofrequency (RF) microneedling technologies have shown effectiveness in treating skin laxity and wrinkles. We report the first experience using a novel device with 1‐mm long ultrathin electrodes that utilizes a smooth RF‐assisted ablation mode.
Objective: To evaluate the safety and effectiveness of treatment with a fractional RF device using 1.0‐mm long × 0.15‐mm diameter ultrathin electrode tips for improvement of facial skin texture and wrinkles.
Methods and Materials: This was a prospective, open‐label, intraindividual‐controlled trial. Nine participants (mean age: 47.6, Fitzpatrick skin type II–IV, Fitzpatrick Elastosis Wrinkle Scale [FEWS] score: 3–6) underwent six treatment sessions with a fractional RF technology utilizing an array of 6 × 6 1‐mm long ultrathin electrodes. Treatment effectiveness was assessed by FEWS and the Global Aesthetic Improvement Scale (GAIS). Safety and tolerance were evaluated.
Results: Three months after the sixth treatment session, blinded, investigator‐assessed FEWS decreased from baseline 4.33 ± 0.67–3.33 ± 0.67 (p < 0.005); 88.9% of participants showed overall skin improvement using the physician‐assessed GAIS, and all of the participants reported improvement in skin texture and wrinkles. Treatment was well tolerated, with no adverse events and no downtime. Histological analysis in a porcine model showed a fractional pattern of epidermal ablation and dermal coagulation with intervening zones of normal healthy tissue. These changes were followed by progressive epithelialization over a period of 13 days.
Conclusion: The fractional RF technology with the novel 1.0 long × 0.15 mm ultrathin electrodes tips was effective in improving skin texture and wrinkles without impacting the participants’ daily activities.
KEYWORDS
Fractional, Photodamage, Radiofrequency, RF face slimming, skin rejuvenation devices, resurfacing, skin texture, eye skin tightening treatment device
INTRODUCTION
The increase in life expectancy coupled with the growing demand for youthful appearing skin has increased the de-mand for effective facial cosmetic treatments, particularly for noninvasive, nonsurgical, low‐risk skin rejuvenation treat-ments with minimal risk and downtime. Aging is associated with morphological changes in the skin that are caused by declining fibroblast numbers, and reduced concentrations of collagen, elastin, and glycosami-noglycan (GAG) biosynthesis. These changes lead to skin laxity, texture change, and wrinkle formation.1
In recent years, skin rejuvenation using radiofrequency
(RF) has gained popularity. Fractional RF technologies,using insulated or noninsulated microneedles that penetrate the skin, cause partial destruction of the epidermis followed by its regeneration. The RF energy generated by the mi-croneedles heats the superficial and deep dermis, creating zones of clinically imperceptible thermal microwounds be-tween areas of normal healthy skin and triggers the wound healing cascade.2,3 Zones of normal, untreated skin promote new collagen, elastin, and (GAG) formation, resulting in improved skin texture, wrinkle reduction, tightening, and lifting.4–13
The VoluDerm™ technology (Legend Pro™; Lumenisl) is a fractional RF technology indicated for noninvasive dermatological procedures requiring skin ablation and res-urfacing. The disposable tip consists of a high‐density array of ultrathin electrodes which smoothly and effortlessly glide into the epidermis by producing continuous ablation at 1 MHz (referred to as “RF penetration assist [RF‐PA]), in lieu of a mechanical mechanism which can be painful. With RF technologies that use a mechanical mechanism for skin penetration, the RF needles puncture the skin using me-chanical force, and the RF is only emitted after needle pe-netration. With the novel RF‐PA, the penetration is facilitated via RF pulse which creates an ablative channel, easing penetration, without the use of force.
The ultrathin electrodes cause pinpoint‐sized ablation in the dermis and surrounding coagulation which induces a wound healing response with the production of collagen, elastin, and GAGs to strengthen and volumize the skin. The safety and effectiveness of fractional RF ultrathin electrodes on skin texture, laxity, and wrinkle reduction were demon-strated using electrode tip arrays of 6 × 6 ultrathin 0.6‐mm long electrodes (gen36 tips, Voluderm; Lumenis).14 In this study, we evaluated the safety and effectiveness of this RF technology with a 6 × 6 array of longer, ultrathin electrodes, 1.0 mm in length and 0.15 mm in diameter (gen 36L tips), for improvement of facial skin texture and wrinkles.
MATERIALS AND METHODS
Design and subjects
This was an institutional review board single‐center, prospective, open‐label, intraindividual controlled trial. The study population included healthy adults aged 30–50 years with Fitzpatrick skin type I–VI who wished
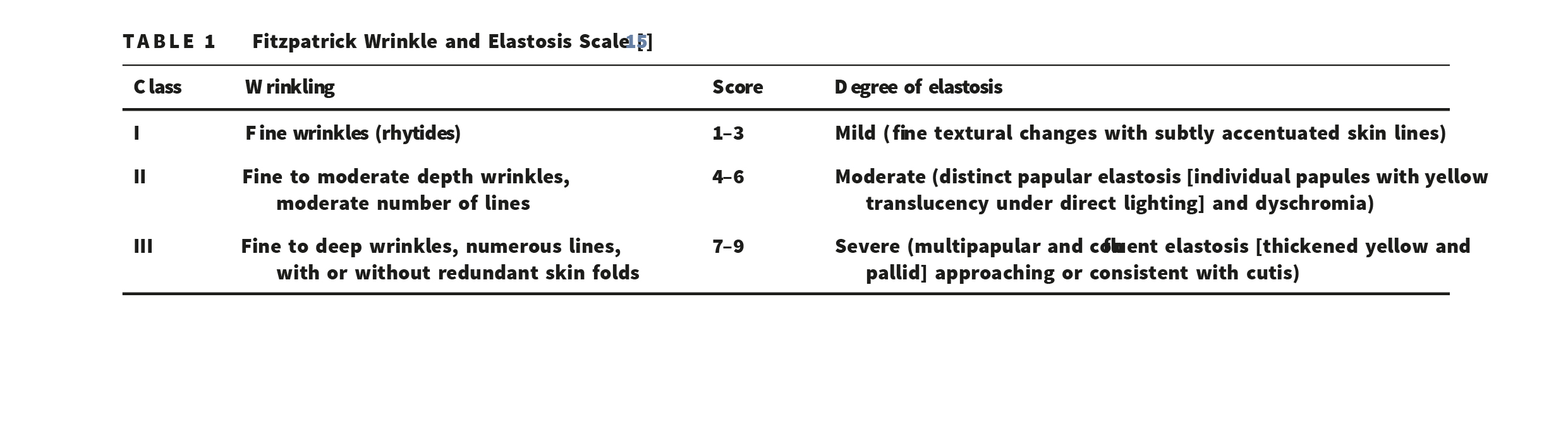
TABLE 1 Fitzpatrick Wrinkle and Elastosis Scale [15] to improve the appearance of their skin wrinkles and texture and had at least two facial subareas with visible wrinkles (Fitzpatrick Elastosis Scale [FEWS] score 3–6).15 The exclusion criteria included implantable elec-tronic devices that could be disrupted by RF energy, active dermatological disorders, severe concurrent con-ditions or an impaired immune system, use of medica-tions that could affect healing, recent treatments of the face or neck with fillers, botulinum toxin, implants, threads and surgery, pregnancy or breastfeeding (Table 1).
Treatment timeline
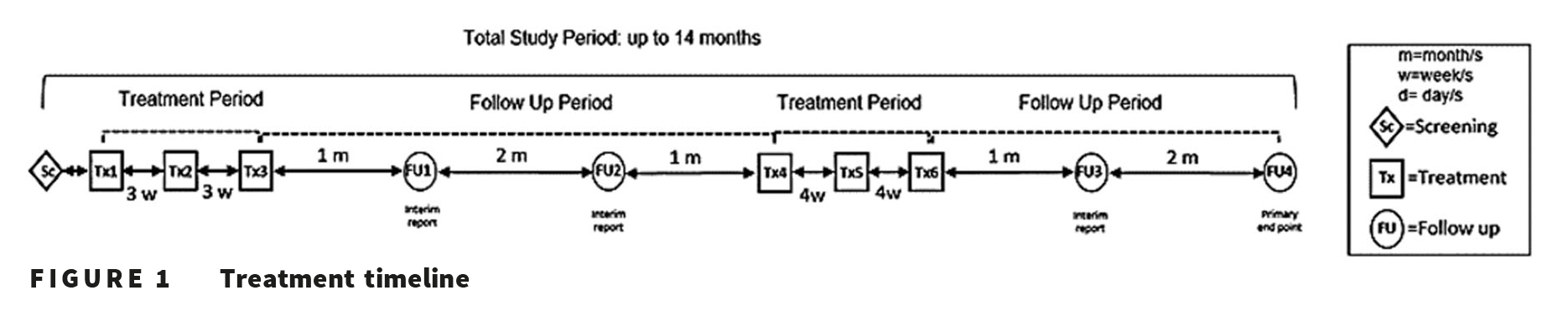
Each study participant received six treatments using the Legend Pro System (Lumenis). The first three treatments were administered at 3‐week intervals, with 1‐ and 3‐month follow‐up visits. An additional three, treatments were performed at 4‐week intervals after the initial 3‐month follow‐up visit, followed by another 1‐ and 3‐month follow‐up visit (Figure 1).
The entire face, including the perioral and peri-orbital regions, was treated. Before each treatment, the treatment area was cleaned and dried. Patients had the option to use a topical anesthetic agent (lidocaine 2.5% + prilocaine 2.5% ointment), which was applied for 30 min before treatment and removed before treat-ment commenced.
Treatment protocol
During the first three sessions, low (10% energy level with 15% exposure rate) to medium (20% energy level with 25% exposure rate) preset parameters were used. For the first treatment session, a single pass over the treatment area (with no overlap) was performed. In the second treatment session, a single pass with 50% overlap was performed, and in the third treatment session, two passes were performed. In the fourth to sixth treatment sessions, two passes were performed at medium (20% energy level with 25% exposure rate) to high (30% energy level with 25% exposure rate) preset parameters. The parameters could be lowered at the treating physician’s discretion to ensure patient comfort.
Subjects were instructed to use a mild cleanser with tepid water and apply a moisturizer (Ciclafate, Avene) for 48 h after treatment. A broad spectrum, mineral sunscreen, SPF 50, was used throughout the duration of the study.
Outcome measures
At baseline and at the follow‐up visits, the treatment area was photographed using standardized conditions (Intellistudio; Canfield Scientific).
The investigator and subjects used the Global Aesthetic Improvement Scale (GAIS) to independently grade the change in skin appearance from baseline to the follow‐up visits at 1 and 3 months after the third treatment session and 1 and 3 months after the last treatment session (0 = worse, 1 = no change, 2 = improved, 3 = much improved, 4 = very much improved). The investigator and subjects in-dependently graded the skin’s improvement by comparing the subject’s visual and photographic appearance at follow‐up against an archival photograph taken at baseline. Changes in skin texture and wrinkles were evaluated by the FEWS by blinded evaluation of standardized photographs taken at baseline, 1‐ and 3‐month follow‐up visits. Treatment safety was assessed by the incidence of expected treatment‐related skin response (i.e., erythema and edema) and any adverse events that occurred fol-lowing the treatments (blistering, crusting, changes in pigmentation, scarring). The duration of downtime, de-fined as the period following the procedure during which the subject felt unable or unwilling to go out in public, was also assessed.
Study endpoints
The primary endpoint of the study was blinded, physician‐assessed improvement in the treatment area of at least 1 point on the FEWS at 3 months after the last (sixth) treat-ment session as compared to baseline. The secondary end-point of the study was blinded, investigator‐assessed FEWS improvement at 1 month after the last treatment session as compared to baseline. Additional endpoints were (a) investigator‐assessed improvement of skin texture and wrinkles according to the GAIS; (b) the improvement of the FEWS from baseline to 3 months after the last treatment sessions, assessed by blinded evaluators using pre‐ and posttreatment photographs, (c) subject‐assessed skin im-provement, satisfaction, and downtime.
Statistical analysis
Statistical analyses were mainly descriptive in nature, with continuous variables summarized by mean and standard deviation, and categorical variables by count and percentage. The difference between baseline and follow‐up was analyzed using t‐test. The level of sig-nificance was 5%.
Porcine histology
Histological analysis was performed using a pig model. Porcineskinwastreatedwithlow,medium, andhighen-ergies using the same RF technology, and allowed to heal up to 13 days after treatment. Skin samples for histological and morphological analysis were collected for the following time points: Immediately after treatment, 3, 6, and 13 days posttreatment. In addition, a control skin sample was col-lected. Serial sections were prepared and stained using he-matoxylin and eosin for histological examination and analysis. Slides were evaluated under a light microscope (Olympus BX53F) and the most representative slide was photographed with a digital camera (Olympus DP72). Dimensions of lesions (depth and width) were measured with a peak scale loupe ×10 micrometer. The measurement was repeated three times.
RESULTS
Ten participants were enrolled in the study; one partici-pant dropped out due to reasons unrelated to the study. A total of nine Caucasian females with Fitzpatrick skin types II–IV and a mean age of 47.6 ± 4.3 years (range: 44–50 years) underwent six treatment sessions with VoluDerm™ technology, with 1‐mm long ultrathin electrodes. The baseline investigator‐assessed FEWS was 4.33 ± 0.67. None of the subjects received pretreatment anesthesia before the first treatment session, three sub-jects (33.3%) received pretreatment anesthesia for 15–20 min before the second treatment session, two subjects (22.2%) received pretreatment anesthesia for
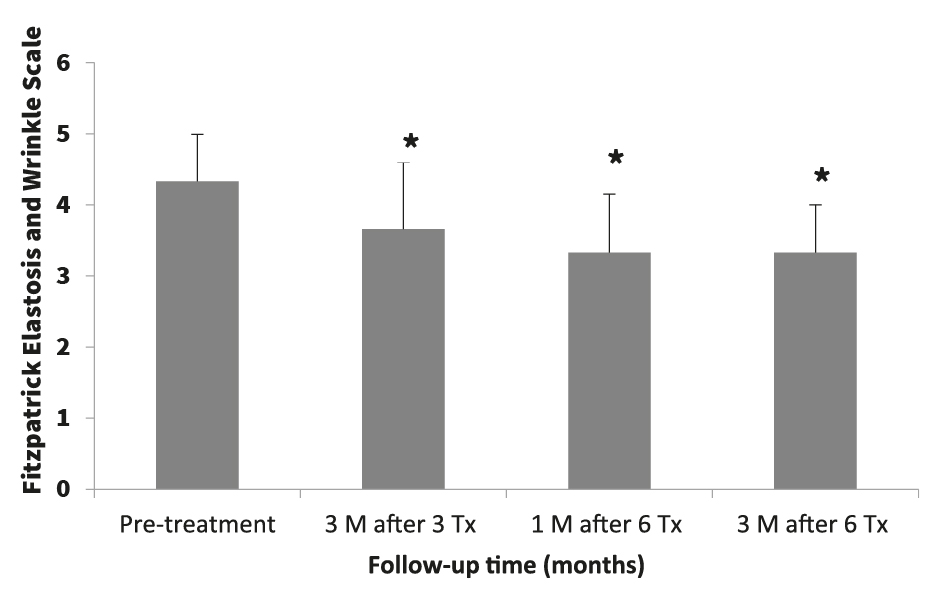
FIGURE 2 The change in Fitzpatrick Elastosis Scale (FEWS) score between baseline (pretreatment) and follow‐up. Bars represent mean FEWS score ± standard deviation; *p < 0.005 for the difference between baseline and each follow‐up time point. M, months; Tx, treatment session
15–20 min before the third, fourth, and fifth treatment sessions, and seven subjects (77.8%) received pretreat-ment anesthesia before the sixth treatment session.
Treatment response
Three months after the last (sixth) treatment session, the change from baseline in mean investigator‐assessed FEWS was 3.33 ± 0.67 points (p < 0.005), thereby achieving the primary endpoint of the study and showing improvement in skin texture and wrinkles (Figure 2). As shown in Figure 2, investigator‐assessed FEWS also showed statistically sig-nificant improvement at 1 month after the last (sixth) treatment session and at 3 months after the third treatment session (3.33 ± 0.82 and 3.67 ± 0.94, respectively; p < 0.005 for both time points).
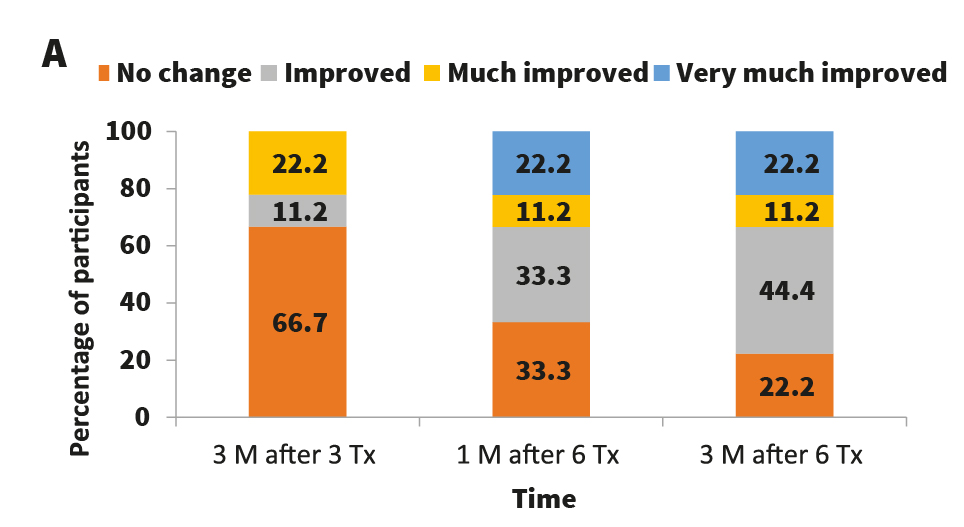
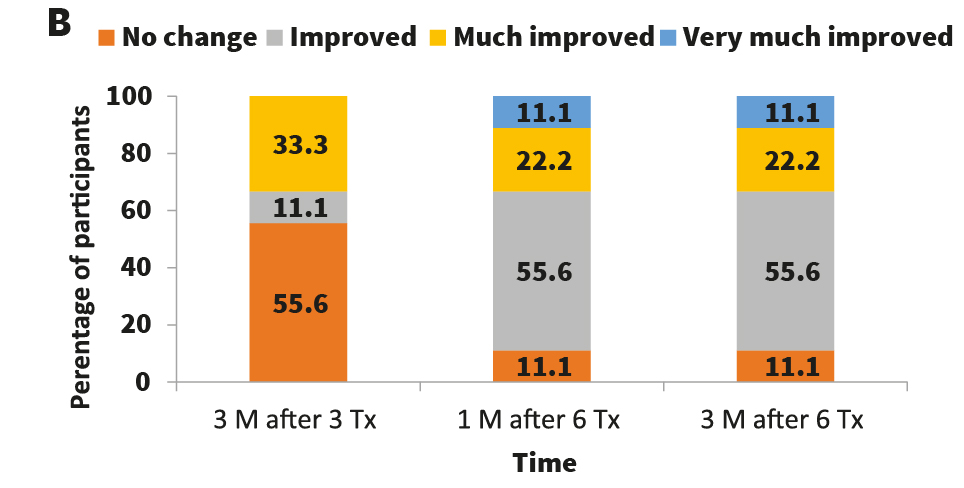
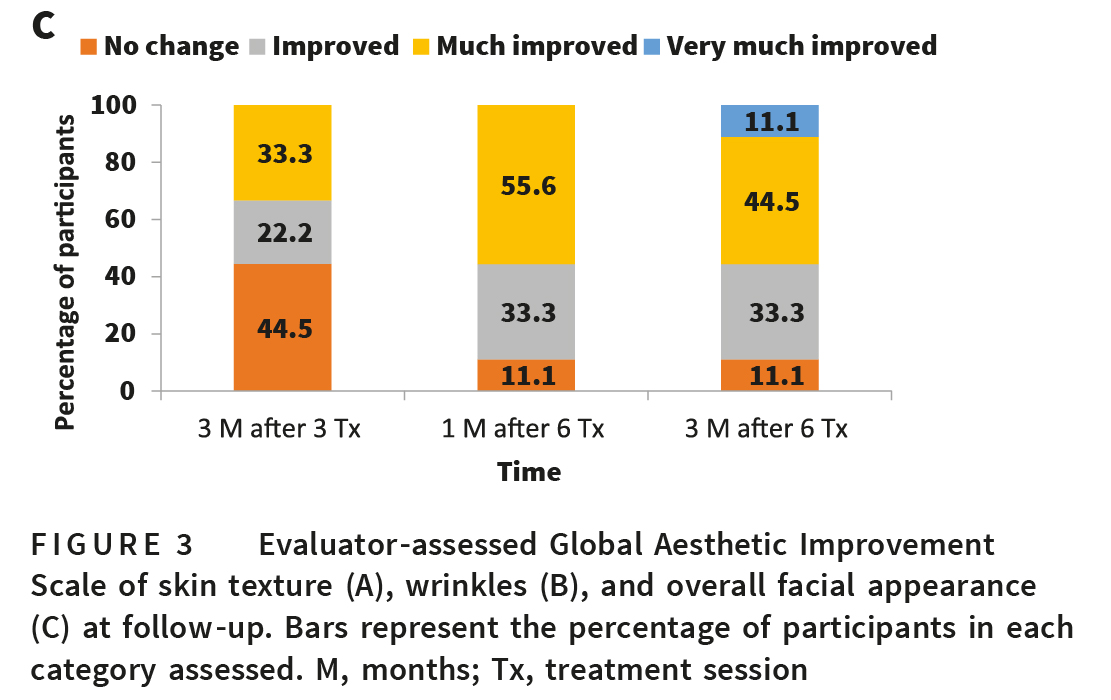
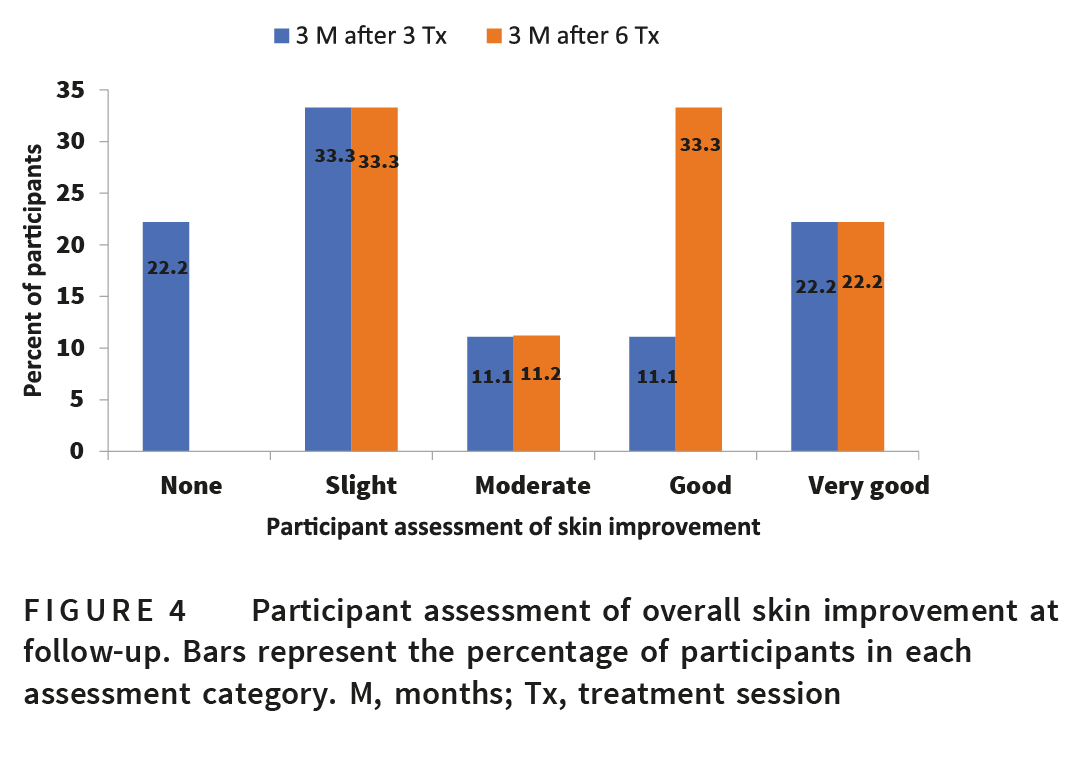
The percentage of patients with improvement in skin texture and wrinkles increased over time, as did the ex-tent of improvement (Figure 3). Three months after the last (sixth) treatment session, eight subjects (88.9%) were evaluated by the investigator as showing overall skin improvement according to GAIS. Wrinkles improved in five subjects (55.6%), much improved in two subjects (22.2%), and very much improved in one subject (11.1%). Skin texture improved in four subjects (44.4%), much improved in one subject (11.1%), and very much im-proved in two subjects (22.2%). Three months after the third treatment session, seven subjects (77.8%) reported various degrees of improvement in skin texture and wrinkles, and 3 months after the last treatment session, all of the subjects reported improvement in their skin texture and wrinkles (Figure 4).
Representative “before and after” photographs showing improvement following six treatment sessions are shown in Figure 5. Visible improvement in skin tex-ture, pore size, skin color, and wrinkles were observed. Incidentally, very good improvement in acne scars was also noted in one subject (Figure 5A,B).
Safety
Treatments were well tolerated. Immediate postprocedure
reactions included erythema and/or edema. No other
Before and after RF Wrinkle Treatments
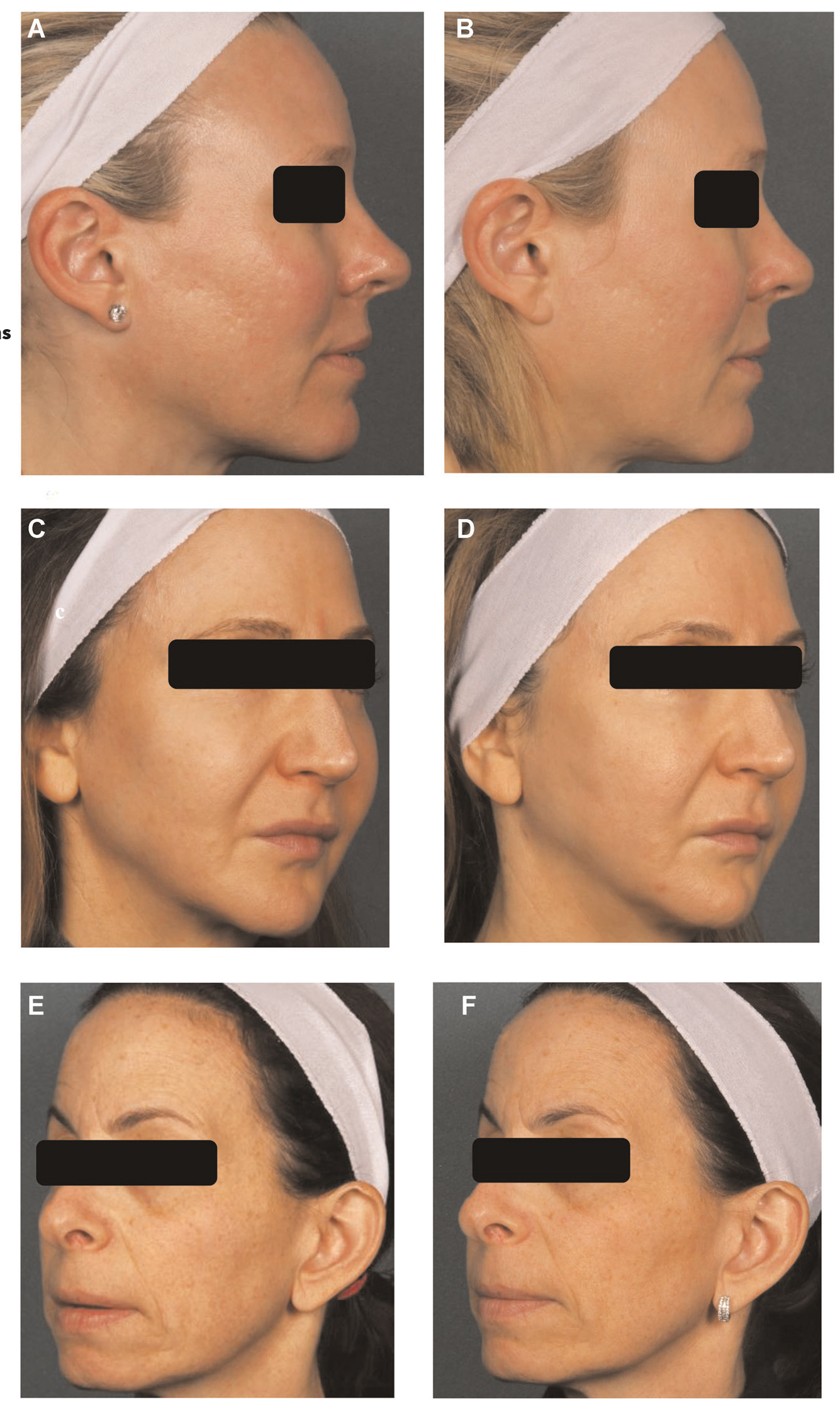
FIGURE 5 Representative “before and after” photographs, showing the improvement in skin texture following treatment with the system.
(A, B) A 44‐year‐old woman before treatment (A) and showing significant improvement in skin texture and acne scars 3 months after the last
(sixth) treatment session (B). (C, D) A 45‐year‐old woman before treatment (C) and showing significant improvement in skin texture and nasolabial folds 3 months after the last (sixth) treatment session (D). (E, F) A 59‐year‐old woman before treatment (E) and showing significant improvement in skin texture and wrinkles 3 months after the last (sixth) treatment session (F)
adverse events were reported. No downtime was reported for any of the subjects and they all felt comfortable going out in public.
Porcine histology
Histological evaluation was performed in a porcine model. These samples were treated with the same novel RF technology (kindly provided by Lumenis) and showed that application of the RF‐PA ultrathin 1‐mm long electrodes to the skin induced a fractional pattern of epidermal ablation and dermal coagulation with inter-vening zones of normal healthy tissue. These changes were followed by progressive epithelialization over a period of 13 days. Specifically, treatment with low or high settings showed partial epidermal necrosis at the ablation zones to depths of approximately 1200 μm and surrounding coagulation zones of approximately 150 μm and a mild lymphocytic infiltrate which lasted for up to
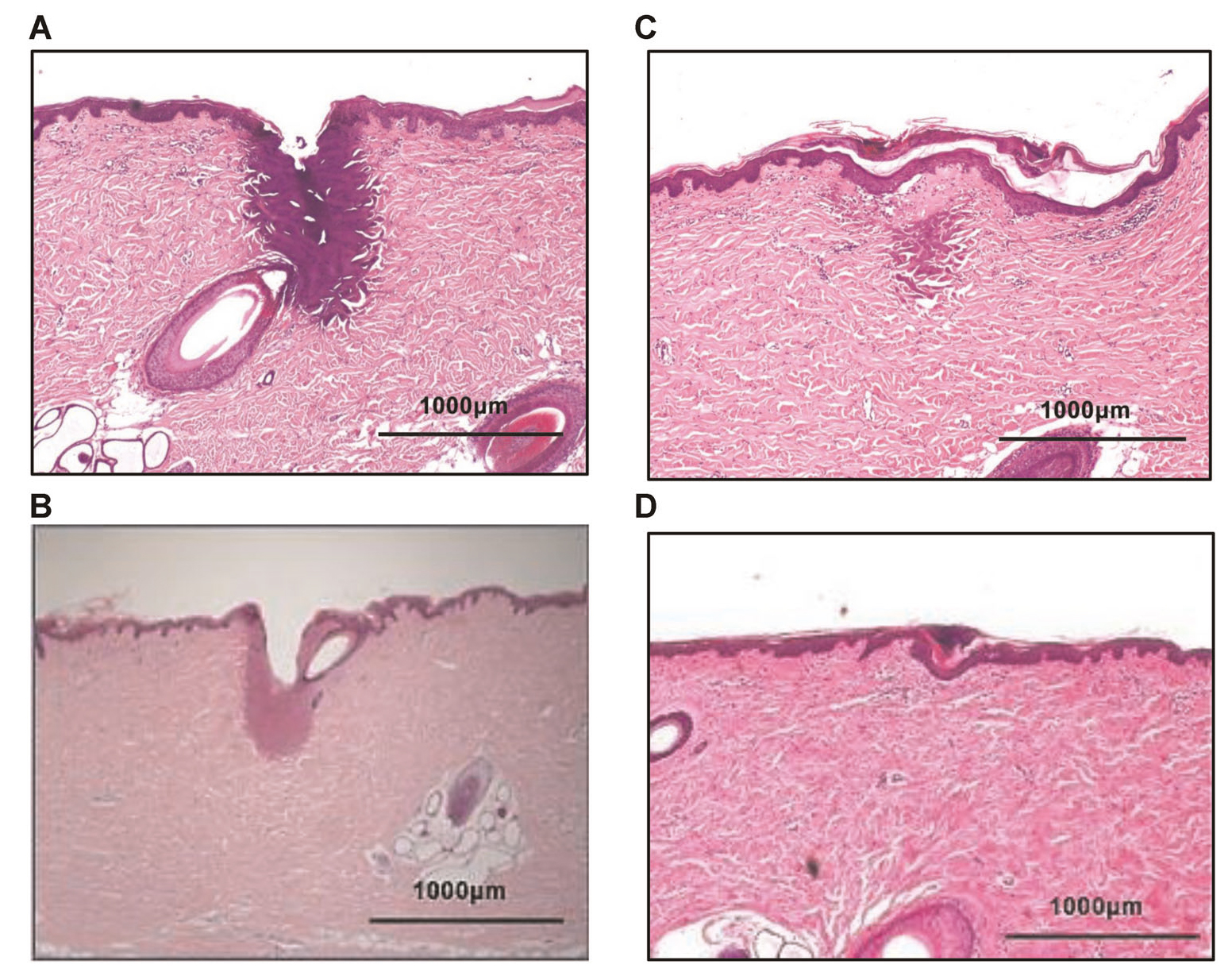
FIGURE 6 Histological analysis of porcine skin after treatment with a high‐level setting. (A) Immediately after treatment: Ablated channel corresponding to RF needle insertion, measuring approximately 1200 μm in depth, a surrounding coagulation zone of approximately 150 μm and a mild lymphocytic infiltrate; (B) Three days after treatment: Evidence of scale crust, partial epithelialization, and a and a mild lymphocytic infiltrate; (C) 6 days after treatment: Regeneration of the epidermis, scale crust, minimal residual coagulative change in the dermis and a mild lymphocytic infiltrate; (D) Thirteen days after treatment: Epidermis has epithelialized and fibrosing granulation tissue is present in the treated areas of skin, along with a mild lymphocytic infiltrate. Figure provided courtesy of study sponsor
3 days after treatment (Figures 6A,B and 7A,B). Six days after treatment with low or high settings the skin samples showed a regenerating epidermis, residual coagulative change, and healed wounds, with mild lymphocytic in-filtrate (Figures 6C and 7C).
DISCUSSION
This study demonstrated that six consecutive treatment sessions for skin rejuvenation and wrinkles using an ar-ray of RF‐PA ultrathin electrodes with a novel 1‐mm disposable tip was well tolerated, with no downtime or adverse events. The treatment significantly improved skin texture and wrinkles after three treatment sessions at low to medium energy settings, and the extent of improve-ment in skin texture and wrinkles increased after three additional treatment sessions at medium to high‐energy settings, lasting for at least 3 months after the last treatment session. The majority of treatments were per-formed without the need for topical anesthetic cream. Anesthetic cream (5% lidocaine/prilocaine) was applied only at the request of the patients. None of the subjects had anesthetic cream for the first session. Three subjects received topical anesthetic before the second treatment, two patients before the third, fourth, and fifth treat-ments, and seven subjects received topical anesthesia before the sixth and final treatment. Treatment para-meters were slowly advanced from one pass at low preset settings for the first session to two passes at medium to high preset settings. The greater need for anesthesia during the last treatment was likely due to the use of more aggressive treatment parameters. Notwithstanding, two subjects completed all the sessions without any to-pical anesthetic.
The extent of dermal change observed reflected the en-ergy setting. At the low energy setting, the depth of ablation was shallower and zones of coagulation were smaller than at the higher energy settings. There was a correspondingly larger zone of fibrosing granulation tissue evident in the high‐energy treated samples. The histological analysis in porcine skin corroborates other reports, which showed that RF microneedling at various energy levels triggers a natural wound healing response with complete healing occurring within a 2‐week period.16 Dermal RF‐induced coagulation caused mixed cellular infiltration, neovascularization, and granulation tissue formation,17 blood vessel response,16 in-crease in mid to deep dermis GAGs, increased epidermal mitotic index,18 and increased epidermal hyaluronan and CD44 expression.19
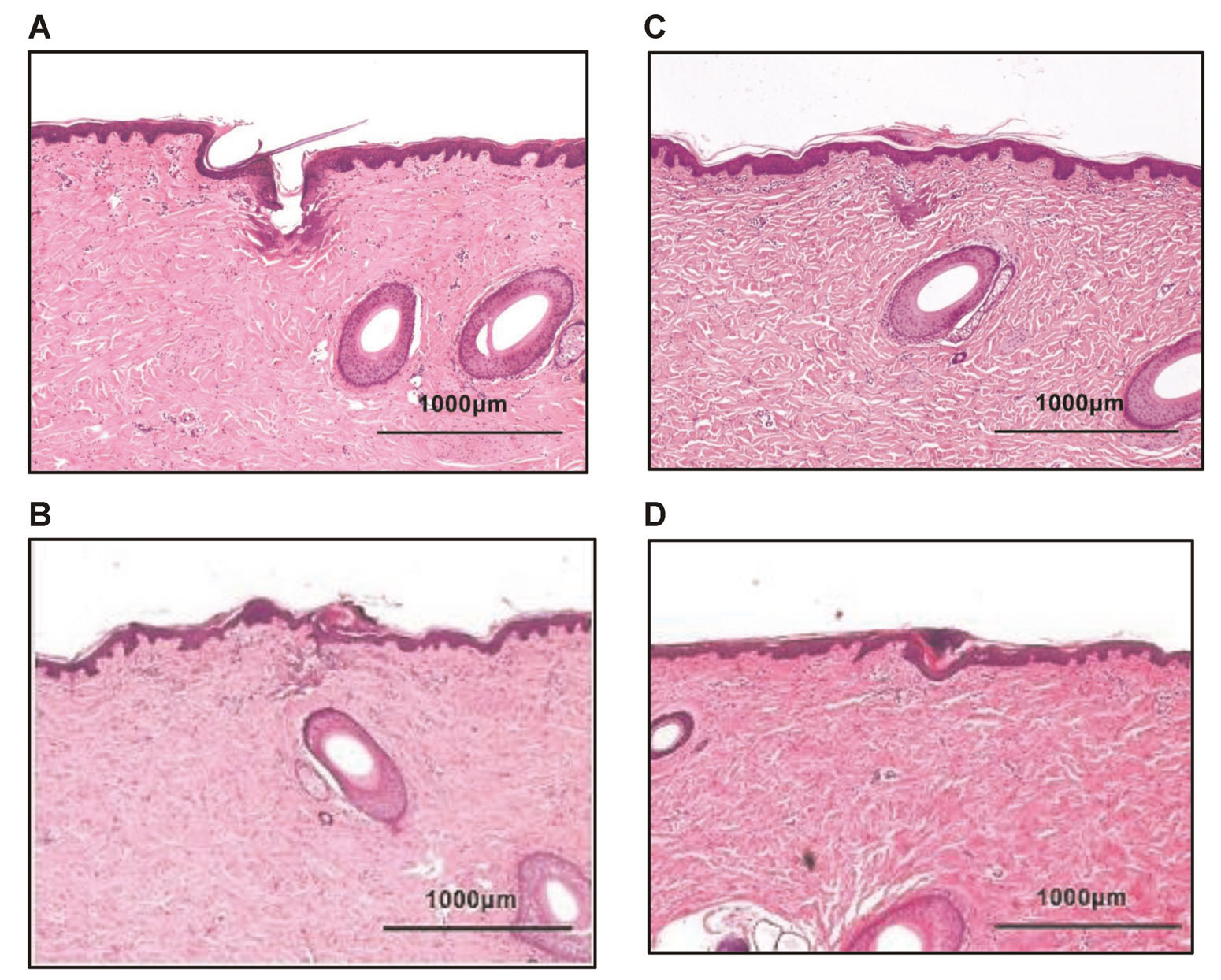
FIGURE 7 Histological analysis of porcine skin after treatment with a low‐level setting. (A) Immediately after treatment: Ablated channel corresponding to RF needle insertion, measuring approximately 600 μm in depth, a surrounding coagulation zone of approximately 70 um and a mild lymphocytic infiltrate; (B) Three days after treatment: Evidence of scale crust, partial epithelialization and a and a mild lymphocytic infiltrate; (C) 6 days after treatment: Regeneration of the epidermis, scale crust, minimal residual coagulative change in the dermis and a h mild lymphocytic infiltrate; (D) Thirteen days after treatment: Epidermis has epithelialized and fibrosing granulation tissue is present in the treated areas of skin, along with a mild lymphocytic infiltrate. Figure provided courtesy of study sponsor
Other clinical studies with a similar number of treatment sessions have demonstrated that RF‐microneedle technolo-gies were effective for treating skin laxity and wrinkles.4,5,8–13 The fractional RF technology reported on in this study produces focal ablation of columnar volumes of tissue to a depth of approximately 1200 μm with a zone of residual surrounding coagulation measuring approximately 150 μm. Many of the fractional RF devices use a mechanical insertion process which contributes to the treatment dis-comfort. The technology we report on using RF energy to ablate the epidermis during electrode insertion into tissue (RF‐PA), which allows a smooth and barely perceptible penetration into the skin. Insertion pain is further lessened by using ultrathin, 0.15‐mm diameter electrode pins. More-over, as the ultrathin electrodes are not insulated, the RF energy is emitted along the entire length of the needle, re-sulting in effective coagulation, bulk volumetric heating, and no bleeding.20 These findings are more pronounced with the longer 1‐mm electrodes used in the current study, as com-pared with the previously described experience with the 0.6‐mm electrodes. Nonmechanical insertion also reduces the incidence of adverse events such as bleeding and posttreat-ment hyperpigmentation.21
The study’s limitations include its open‐label design and small sample size. However, both investigator‐assessed and subject‐assessed results indicate that treatment with the RF‐PA ultrathin electrodes was effective in improving skin tex-ture and wrinkles. Although not an intended outcome of the study, the treatment also improved the acne scars of one subject. The effectiveness of treatment was notable at three months after the last treatment session, indicating a durable effect. Importantly, treatment with the RF‐PA ultrathin electrodes provided effective facial rejuvenation without impacting the participants’ daily activities. Studies in a larger patient population are warranted to confirm the results.
ACKNOWLEDGMENT
This study has been supported by a research grant from Lumenis.
ORCID
Arielle N. B. Kauvar
REFERENCES
1. Uitto J. The role of elastin and collagen in cutaneous aging: intrinsic aging versus photoexposure. J Drugs Dermatol. 2008;7:s12–6.
2. Arnoczky SP, Aksan A. Thermal modification of connective tis-sues: basic science considerations and clinical implications. J Am Acad Orthop Surg. 2000;8:305–13.
3. Dierickx CC. The role of deep heating for noninvasive skin re-juvenation. Lasers Surg Med. 2006;38:799–807.
4. Hantash BM, Ubeid AA, Chang H, Kafi R, Renton B. Bipolar fractional radiofrequency treatment induces neoelastogenesis and neocollagenesis. Lasers Surg Med. 2009;41:1–9.
5. Hantash BM, Renton B, Berkowitz RL, Stridde BC, Newman J.Pilot clinical study of a novel minimally invasive bipolar micro-needle radiofrequency device. Lasers Surg Med. 2009;41:87–95.
6. Hruza G, Taub AF, Collier SL, Mulholland SR. Skin rejuvena-tion and wrinkle reduction using a fractional radiofrequency system. J Drugs Dermatol. 2009;8:259–65.
7. Gold MH, Adelglass J. Evaluation of safety and efficacy of the TriFractional RF technology for treatment of facial wrinkles. J Cosmet Laser Ther. 2014;16:2–7.
8. Seo KY, Yoon MS, Kim DH, Lee HJ. Skin rejuvenation by mi-croneedle fractional radiofrequency treatment in Asian skin; clinical and histological analysis. Lasers Surg Med. 2012;44:631–6.
9. Seo KY, Kim DH, Lee SE, Yoon MS, Lee HJ. Skin rejuvenation by microneedle fractional radiofrequency and a human stem cell conditioned medium in Asian skin: a randomized controlled in-vestigator blinded split‐face study. J Cosmet Laser Ther. 2013;15: 25–33.
10. Lee HS, Lee DH, Won CH, Chang HW, Kwon HH, Kim KH, et al. Fractional rejuvenation using a novel bipolar radiofrequency system in Asian skin. Dermatol Surg. 2011;37:1611–9.
11. Gold M, Taylor M, Rothaus K, Tanaka Y. Non‐insulated smooth motion, micro‐needles RF fractional treatment for wrinkle re-duction and lifting of the lower face: international study. Lasers Surg Med. 2016;48:727–33.
12. Tanaka Y. Long‐term three‐dimensional volumetric assessment of skin tightening using a sharply tapered non‐insulated microneedle radiofrequency applicator with novel fractionated pulse mode in Asians. Lasers Surg Med. 2015;47:626–33.
13. Alexiades‐Armenakas M, Rosenberg D, Renton B, Dover J,Arndt K. Blinded, randomized, quantitative grading com-parison of minimally invasive, fractional radiofrequency and surgical face‐lift to treat skin laxity. Arch Dermatol. 2010;146: 396–405.
14. Shapiro S. VoluDerm micro‐needle technology for treating skin laxity and wrinkles‐initial clinical experience. Jacobs J Exp Dermatol. 2015;1:006.
15. Fitzpatrick RE, Goldman MP, Satur NM, Tope WD. Pulsed carbon dioxide laser resurfacing of photo‐aged facial skin. Arch Dermatol. 1996;132:395–402.
16. Gershonowitz A, Gat A. VoluDerm microneedle technology for skin treatments‐in vivo histological evidence. J Cosmet Laser Ther. 2015;17:9–14.
17. Zheng Z, Goo B, Kim DY, Kang JS, Cho SB. Histometric ana-lysis of skin‐radiofrequency interaction using a fractionated mi-croneedle delivery system. Dermatol Surg. 2014;40:134–41.
18. Boisnic S, Branchet MC. Ex‐vivo study of hybrid energy technology using a human skin model. Eur J Dermatol. 2014;24:46–52.
19. Lee HJ, Seo SR, Yoon MS, Song JY, Lee EY, Lee SE. Micro-needle fractional radiofrequency increases epidermal hyaluronan
and reverses age‐related epidermal dysfunction. Lasers Surg Med. 2016;48:140–9.
20. Tanaka Y. Treatment of skin laxity using multisource, phase‐controlled radiofrequency. In: Dermatologic surgery and proce-dures, London, UK: InTech; 2017. p. 175–92.
21. Harth Y, Elman M, Ackerman E, Frank I. Depressed acne scars—effective, minimal downtime treatment with a novel
smooth motion non‐insulated microneedle radiofrequency tech-nology. J Cosmet Dermatol Sci App. 2014;4:212–18.