ORIGINAL RESEARCH REPORT Treatment of abdominal cellulite and circumference reduction with radiofrequency and dynamic muscle activation
Abstract
Background: Cellulite is a frequent skin condition for which treatment remains a challenge. A wide variety of treatments are available but most procedures offer suboptimal clinical effect and/or delayed therapeutic outcome. Only few therapeutic options have proven efficacy in the treatment of cellulite. Objective: To determine the efficacy and the safety profiles of radiofrequency and dynamic muscle activation technology in treatment of abdominal cellulite and circumference reduction. Methods: Twenty-five females with abdominal cellulite received 6 weekly radiofrequency and dynamic muscle activation treatments. Treatment areas included the abdomen and both sides of flanks. Subjects were evaluated using standardized photographs, and measurements of body weight and abdominal circumference at baseline, before every treatment visit, and 1 week and four weeks after the final treatment. Subcutaneous tissue thickness was recorded by ultrasound at baseline and 4 weeks after completion of treatment protocol. Physicians’ evaluation and patient’s satisfaction of clinical improvement were also measured. Results: All subjects completed the treatment protocol and attended every follow-up visits. There was significant abdominal circumference reduction of 2.96 and 2.52 cm at 1-, and 4-week follow-up visits (p 0.05), respectively. At four weeks after the last treatment, the average circumference reduction was sustained. Most of the patients were rated to have 25–49% improvement at 5th treatment, and 1- and 4-week follow-up visits. Ninety-two percent of the patients were satisfied with the treatment outcome. Conclusions: Radiofrequency provided beneficial effects on the reduction of abdomen and cellulite appearance. The benefit of muscle activation is yet to be determined.
Key Words: cellulite, dynamic muscle activation, radiofrequency, skin tightening
Introduction Cellulite is a common condition characterized by an irregular, dimpling of the skin, which is mainly found on the thighs, buttocks, and abdomen of postpubertal women (1). The cause of cellulite remains unknown but its etiology is considered multifactorial, including structural, genetic, and endocrine abnormalities. It is evident that weakened connective tissues, enlarged fat cells, and diminished microcirculation play key roles in the pathophysiology of cellulite (2,3). A variety of topical preparations, massage-based therapies, and surgical procedures, including subci-sion and liposuction have been employed to improve the cellulite by promoting microcirculation in the affected areas, loosening the fibrous septae of the subcutaneous tissue, and stimulating the lymphatic drainage (4). However, most procedures offer suboptimal and inconsistent clinical effects and/or a delayed therapeutic outcome (5).
Skin Radiofrequency (RF) device alone and combined RF and light source technologies have been introduced for tissue tightening by volumetric heating of the deep dermis and become one of the most effective treatment modalities for the treatment of cellulite (6,7). Previous studies reported beneficial effects of monopolar (8) and bipolar RF (9,10) in the treatment of cellulite and skin tightening. Monopolar RF provides deep dermal heating but the procedure is 2 R. Wanitphakdeedecha et al. painful, with a delayed outcome, whereas bipolar RF has a limited depth of tissue heating and is also associated with pain.
Tripolar RF has been introduced as a new technology to produce homogenous and deep volumetric heating of tissue thus combining the effects of monopolar and bipolar RF modalities in one applicator. It is designed to deliver focused RF current into the skin via three electrodes, thus generating heat through resistance in both the dermal and subcutaneous layers. The clinical studies on the treatment of cellulite and striae distense using this technology demonstrated the positive clinical effects with longer-term results over successive treatment sessions without discomfort (11,12).
Recently, the latest technology has resulted in the cellulite reduction, and the treatment of wrinkles by combining of tripolar RF and dynamic muscle activation. The technology is based on three or more electrodes designed to deliver focused RF current combined simultaneously with muscle activation. The RF energy generates heat through resistance in both the dermal and subcutaneous layers. Selective and focused electro-heating of the skin is intended to stimulate collagen remodeling and increase fat metabolism (13). Simultaneously, dynamic muscle activation is proposed to stimulate circulation, venous return, and lymphatic drainage thus resulting in effective oxygenation (See also: Pollogen’s Oxygen therapy treatment device) and removal of metabolic waste by-products. This combined treatment results in body shaping, skin tightening, and improvement of cellulite appearance.
The present study was designed to determine the efficacy and the safety profiles of an RF and dynamic muscle activation technology in treatment of abdom-inal cellulite and circumference reduction. Materials and methods Twenty-five females (age: 24–55 years, mean: 35.5 years) with the presence of more than grade 2 of cellulite (Nurnberger–Muller scale) (14) were recruited to the study. Subjects were instructed to adhere to their regular diet, exercise program, and lifestyle with weight fluctuations not exceeding 2 kilograms from the preceding month. Exclusion criteria included scarring, inflammation or infection of the area to be treated, pregnancy or lactating, subjects with a history of malignancy, implants or a pace-maker device, use of non-steroidal anti-inflammatory drugs or aspirin 2 weeks before and 2 weeks after the treatment, and prior treatment of the area with another method within 1 year of the baseline visit.
All subjects received treatments with an RF and dynamic muscle activation device (Maximus, Pollogen Ltd., Tel Aviv, Israel) once a week for six sessions. After applying a thin layer of glycerin oil on the treatment area, the applicator was employed with slight pressure in a continuous sweeping movement over the skin to simultaneously heat the subcutaneous fat layer and the dermis. RF energy and dynamic muscle activation were firstly administered at RF power of 20 watts, pulse duration of 160 ms, and a frequency of 0.78 Hz to the treatment area of the abdomen and both sides of flanks. The energy levels of RF and muscle activation were adjusted depending on the subjects’ sensitivity and the skin response. During the treatment, heat sensation was regularly monitored verbally and physically. A sensation similar to a warm massage without pain was set as an ideal feeling during the treatment. The applicator was moved more rapidly or the energy level was reduced if an unpleasant feeling was reported by the subject. The desired endpoints of treatment were skin erythema and temperature at the treated area reaching 42°C. The skin temperature was regularly measured using an infrared thermometer (Mini-Temp MT4; Raytek Corp, Santa Cruz, California) every 2–3 min to ensure that the temperature did not exceed 45°C throughout the treatment. The treatment session lasted approximately 30 min (20 min for the abdomen and 10 min for both sides of flanks). Circumference measurements Before each treatment session, 1 week and 4 weeks after the final treatment, measurements of body weight and circumferences of the treatment sites were taken. Circumference measurements were done using one designated tape measure and were always taken at an umbilicus. Ultrasound measurement A real-time scanning image ultrasound (iU22 ultra-sound system, Philips Medical Systems, Bothell, WA) with a multifrequency linear probe (5–17 MHz) was used to measure the distance between the epidermis and the superficial fascia (Camper’s fascia) separating the superficial and deep subcutaneous layer (15) at 5 cm below an umbilicus. The measurements were evaluated at the baseline and the 4th week after completion of treatment. Each measurement was evaluated on 2 planes by a blinded radiologist (N.L.): the first plane was parallel to the long axis of the abdomen and the second plane was perpendicular to the first one. Cellulite condition evaluation Cellulite grading was determined utilizing the four-stage Nurnberger–Muller scale (13). Standardized digital photographs, using consistent patient positioning, camera angling, and lighting, were obtained at baseline, immediately after and 4 weeks after the final treatment. Clinical improvement scores of pre- and post-study digital photographs using a quartile grading scale (0 = no improvement, 1 = 1–24% improvement, 2 = 25–49% improvement, 3 = 50–74% improvement, and 4 = 75–100% improvement) were graded independently by two blinded dermatologists (T.I. and W.M.) at before 5th treatment, and 1 week, and 4 weeks after completion of the treatment protocol.
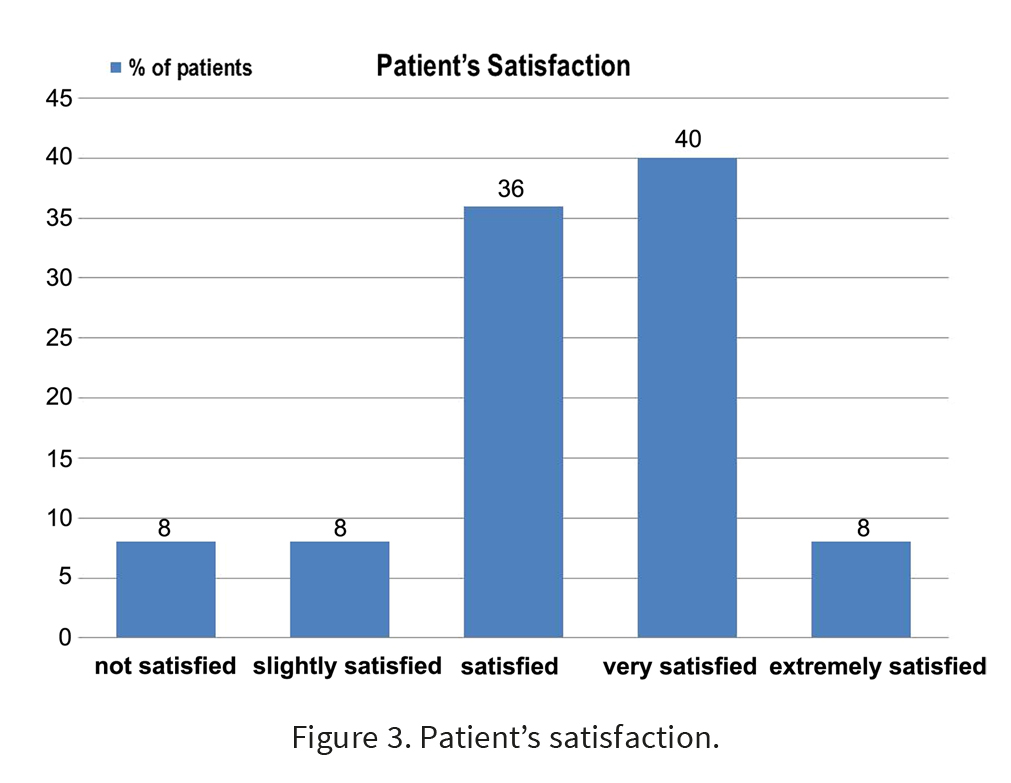
Patients’ satisfaction was also graded at the end of the study using a numerical scale from I to V (I = not satisfied, II = slightly satisfied, III= satisfied, IV very satisfied, and V extremely satisfied). Adverse effects were observed and documented during each treatment session.
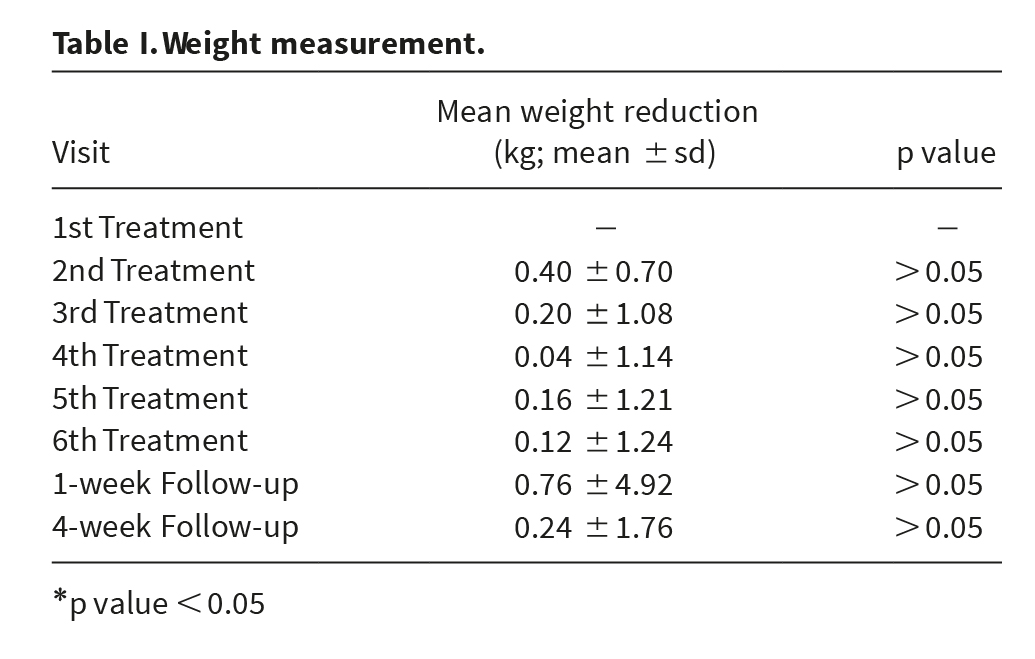
All subjects were instructed to maintain their normal lifestyle, diet, and food consumption during the entire study. No other complimentary treatment including nutritional supplements, mechanical massages, or medication has been given to any subjects. The study protocol was approved by the Ethical Committee on Research Involving Human Subjects, Faculty of Medicine, Siriraj Hospital, Mahidol University. Written informed consent was obtained from all study subjects. Statistical analysis Descriptive statistics including mean, median, minimum, maximum, percentages of circumferential reduction, and 95% confidence interval were used to describe demographic data and circumference measurements. The mean differences of circumference and body weight at pre- and post-treatment were analyzed by a paired-sample t-test. All statistical data analyses were performed using statistical software (SPSS version 16.01; SPSS Inc, Chicago, Illinois). Results All 25 subjects completed the treatment protocol and attended every follow-up visit. The average body weights of all subjects at the baseline, and 1 and 4 weeks after the final treatment were 63.92 = 8.11, 63.16 = 8.08, and 63.68 = 8.14 kg, respectively. No significant body weight reduction, compared with baseline was demonstrated at any follow-up visit (p = 0.26) (Table I).
Immediately after the treatment, the treated skin became warm to the touch, and erythema was observed. The erythema was reported to disappear within 2–3 h after completion of the treatment session by all subjects. Treatment was well tolerated with minimal to no discomfort. The sensation most often described was a mild heating with occasional pinching or slightly tingling. No further adverse
effects, such as postoperative purpura, bullae, crusts, ulcerations, and dyschromia were observed. None of the subjects interrupted the treatment due to pain or discomfort.
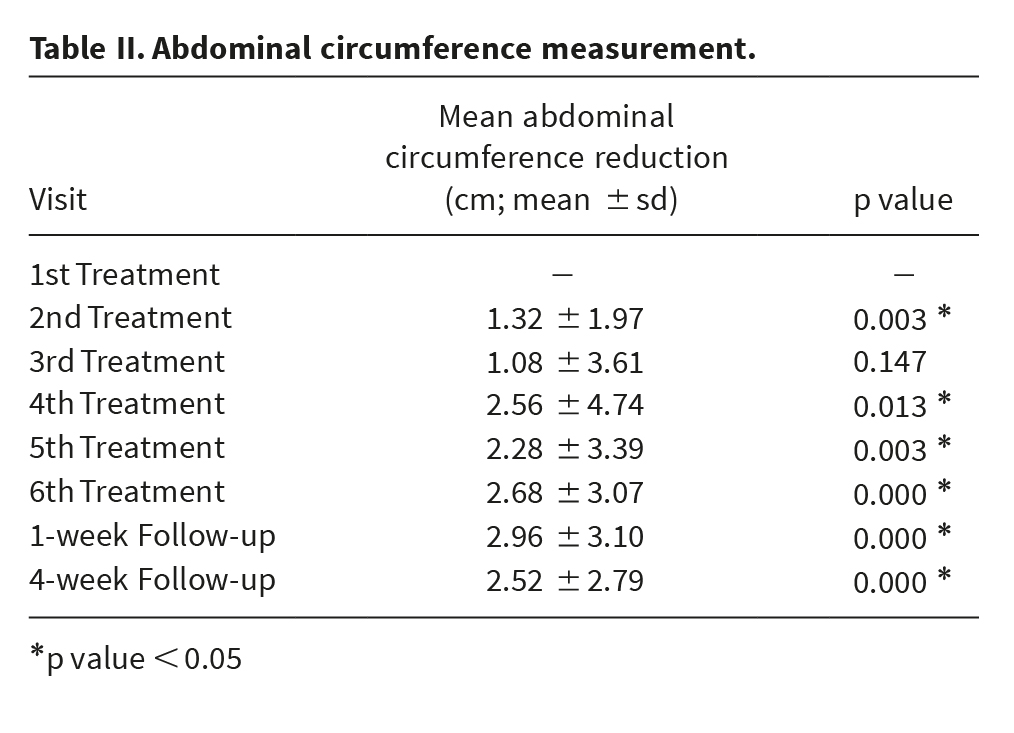
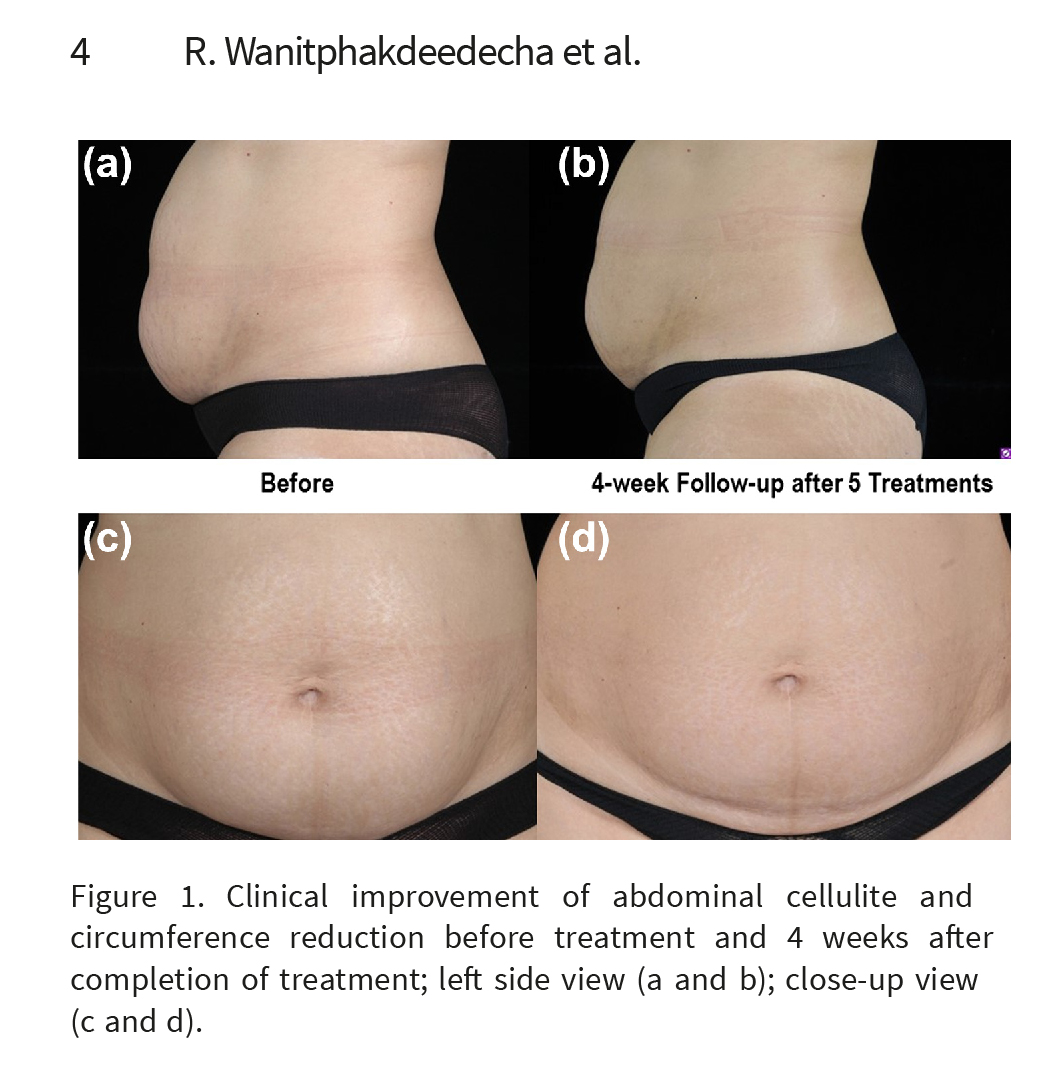
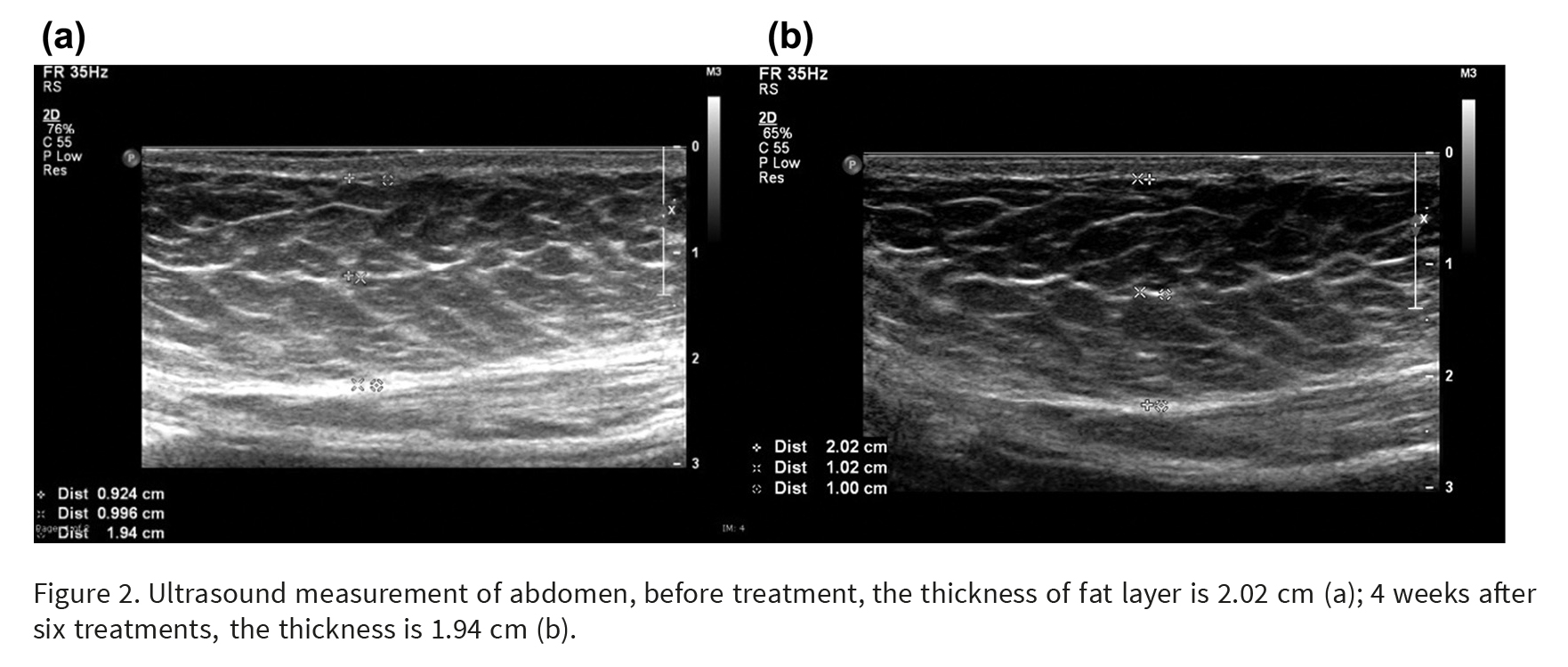
The average abdominal circumference measurement, average reduction, and percentage of reduction are shown in Table II. There was significant abdominal circumference reduction of 2.96 and 2.52 cm at 1- and 4-week follow-up visits (p = 0.05), respectively. Significant reduction of circumferential measurements of the abdomen was seen as early as the 4th treatment visit (after 3 treatments); this significant reduction appeared to be sustained as long as 4 weeks after the treatment was discontinued. In addition, the improvement of striae distense has been noted in most of the patients (Figure 1a–1d). Ultrasound measurements of the distance between the epidermis and the superficial fascia demonstrated that the average thicknesses of abdominal fat before and 4 weeks after completion of treatment were 21.15 = 4.20 mm and 19.98 = 4.45 mm, respectively. The average abdominal fat thickness reduction was 1.17 = 2.22 mm, representing an average reduction of 5.52% of fat thickness. This reduction was found to be statistically significant when compared with the baseline (p = 0.015) (Figure 2).
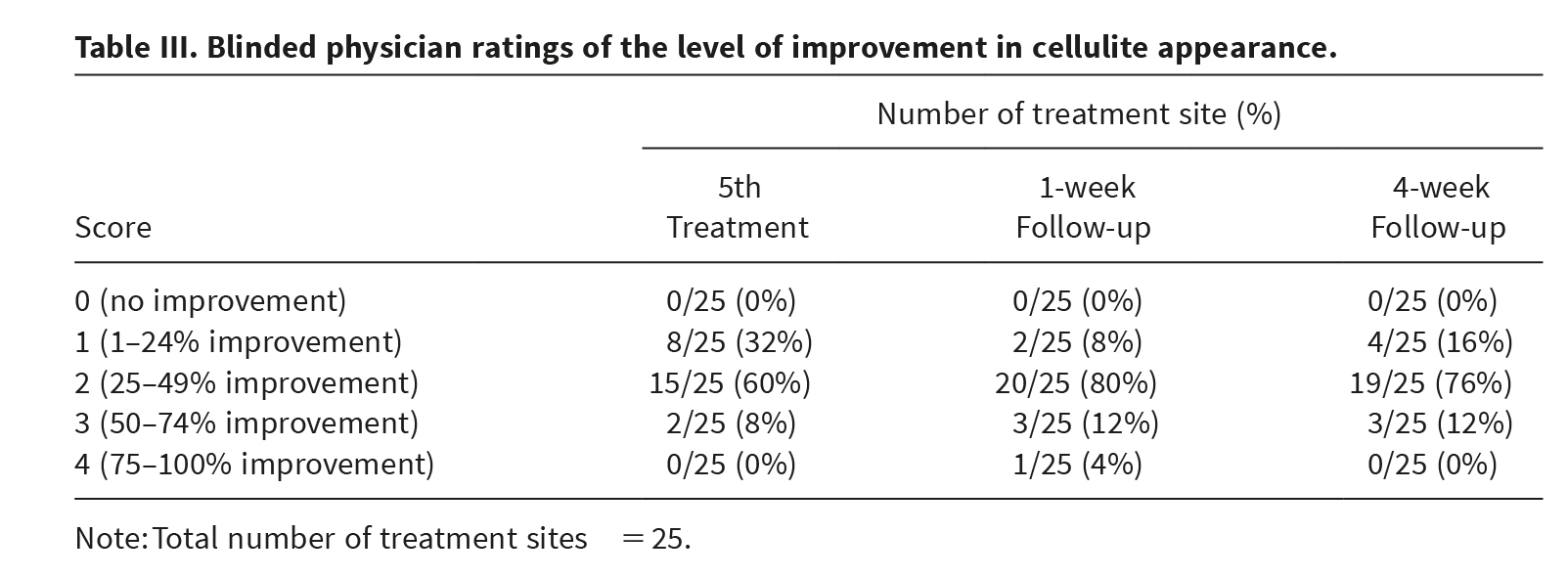
Blinded investigators evaluated the average overall clinical improvement scores of cellulite at before 5th treatment, and 1 week and 4 weeks after the completion of the treatment protocol, which are shown in Table III.
Most of the patients were rated to have improvement score of 2 (25–49% improvement). At the end of the study, patients’ satisfaction was also graded (Figure 3). Ninety-two percent of the patients were satisfied with the treatment outcome.
The adverse effects found in this study were mild and limited to transient erythema, pinching, or slightly tingling sensation during treatment. Of all 150 treatment sessions performed, no serious adverse effects including primary degree burns, blisters, and bruising were observed. Discussion The RF and dynamic muscle activation device is a combined RF and muscle activation system. The RF component of the system is identical to the tripolar RF system which uses a multiple electrode at RF frequency of 1 MHz and maximum power of 50 Watts. The RF energy generates heat through resistance in both the dermal and subcutaneous layers to stimulate collagen remodeling and increased fat metabolism. In addition, no active cooling of the electrodes or the skin is required. Previous clinical studies con-firmed the safety and efficacy of the tripolar RF technology (16,17). Simultaneous with RF, muscle activation is assumed to promote circulation, venous return, and lymphatic drainage resulting in effective oxygenation and metabolic waste by-products elimination. With combination of RF and dynamic muscle activation, the efficacy of the treatment of cellulite appearance, skin tightening, and body shaping is supposed to increase when comparing with the treatment with RF alone.
Manuskiatti et al. (11) evaluated circumference reduction and cellulite treatment with a tripolar RF device in 39 subjects. All subjects received treatments once a week for a total number of eight sessions. A total of 20–28.5 W of RF energy was administered through a tripolar RF electrode configuration at a frequency range of 1 MHz to the treatment area of arms, and those of the abdomen, thighs, and buttocks, respectively. The average abdominal circumference was significantly reduced at 4 weeks follow-up after the last treatment when comparing to baseline was 3.50 = 4.61 cm (p= 0.002).There was a minor reduction in efficacy (less than 1%) between the final treatment and 4 weeks after the final treatment evaluation points but a significant improvement remained.
The average reductions in abdominal fat thickness measured from Manuskiatti’s study and the present study were 0.34 = 2.2 mm (4% reduction) and 1.17 = 2.22 mm (5.52% reduction), respectively. However, the average reduction of subcutaneous fat following RF treatment is much less than that of cryolipolysis (approximately 25.5% reduction at 6 months after a single treatment) which induces apoptosis of fat cell (18). The superior effect in fat thickness reduction found in our study may result from the combination of dynamic muscle activation simultaneously with tripolar RF. The statistically significant fat thickness reduction of 1.17 mm seemed to not be clinically significant and may not be able to explain a total of 2.52-cm reduction in abdominal circumference. However, the abdominal circumference
reduction may result from both fat thickness reduction and skin tightening resulting from RF weekly treatment.
However, the percentages of abdominal circumference reduction at the 4-week follow-up visit found in Manuskiatti’s study and the present study were 3.75% and 2.88%, respectively. The inferior improvement in circumferential reduction of our study may result from the lesser number of treatments. Therefore, the total number of treatments should be increased to 8 sessions to maximize the clinical benefits. In addition, dynamic muscle activation may stimulate abdominal muscle thereby increasing the size of muscle mass (19). Most of the patients in the present study were rated to have 25–49% improvement in their cellulite appearance on the abdominal region. However, the treatment efficacy of RF coupled with dynamic muscle activation on the other anatomical locations need to be further evaluated. Comparing with previous studies (14,16,17) on body contouring response after RF treatment, muscle activation did not provide a significant benefit over RF treatment alone. Well-controlled studies with different treatment parameters and techniques are needed to evaluate the synergistic effect of RF and dynamic muscle activation.
In this present study, most of the patients reported clinical improvement of striae distense. This finding corresponded to the result from a previous study demonstrating that tripolar RF alone also provided a
clinically beneficial effect on improving the appearance of stretch marks (12). The assumption was that collagen remodeling induced by RF heating may be the most likely mechanism that underlies the improvement of the surface appearance of the stretch marks. Moreover, the skin tightening following the RF heating as shown in the previous (11,12) and the present studies may also help shorten the width of the striae, resulting in less visibility of the marks.
In conclusion, circumference and cellulite can be significantly and safely reduced with the use of the RF and dynamic muscle activation technology. The significant circumference reduction could be after 3 treatments and the results appeared to be prolonged as long as 4 weeks after the treatment was discontinued. However, 4 weeks is a very short time for follow-up, especially as the effects appear to drop between the 1-week and 4-week follow-up time. Maintenance treatment may be necessary to maintain improvement. In addition, controlled studies with a larger number of patients and longer follow-up period are warranted to fully evaluate this treatment modality. Acknowledgements This research project is supported by Faculty of Medicine Siriraj Hospital, Mahidol University. The authors wish to thank Mr. Mark E. Manning for his assistance in editing and revising this manuscript, and Ms. Phassara Klamsawat for her assistance in recruiting subjects and managing the database. Author contributions Dr. Wanitphakdeedecha had full access to all of the data in the study and takes responsibility for the integrity of data and the accuracy of the data analysis. Study concept and design: Drs. Wanitphakdeedecha and Manuskiatti
Acquisition of data: Drs. Wanitphakdeedecha, Iamphonrat, Thanomkitti, and Lektrakul
Analysis and interpretation of data: Drs. Wanitphakdeedecha and Thanomkitti Drafting of the manuscript: Dr. Wanitphakdeedecha
6 R. Wanitphakdeedecha et al. Critical revision of the manuscript for important intellectual content: Dr. Manuskiatti
Statistical analysis: Drs. Iamphonrat and Thanomkitti
Obtained funding: none
Administrative, technical, or material support: Dr. Wanitphakdeedecha
Study supervision: Dr. Manuskiatti Financial disclosures Funding/Support: Pollogen™ Ltd.
Role of the Sponsors: the authors received an equipment loan from Pollogen™ Ltd. to use in this study. The authors have no relevant financial interest in this article. Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
References
1. Rossi AB, Vergnanini AL. Cellulite: a review. J Eur Acad Dermatol Venereol. 2000;14:251–262.
2. Avram MM. Cellulite: a review of its physiology and treatment. J Cosmet Laser Ther. 2004;6:181–185.
3. Draelos ZD. The disease of cellulite. J Cosmet Dermatol. 2005;4:221–222.
4. Rao J, Paabo KE, Goldman MP. A double-blinded randomized trial testing the tolerability and efficacy of a novel topical agent with and without occlusion for the treatment of cellulite: a study and review of the literature. J Drugs Dermatol. 2004;3:417–425.
5. Draelos ZD, Marenus KD. Cellulite: etiology and purported treatment. Dermatol Surg. 1997;23:1177–1181.
6. Dierickx CC. The role of deep heating for noninvasive skin rejuvenation. Lasers Surg Med. 2006;38:799–807.
7. Fitzpatrick R, Geronemus R, Goldberg D, Kaminer M, Kilmer S, Ruiz-Esparza J. Multicenter study of noninvasive radiofrequency for periorbital tissue tightening. Lasers Surg Med. 2003;33:232–242.
8. Goldberg DJ, Fazeli A, Berlin AL. Clinical, laboratory, and MRI analysis of cellulite treatment with a unipolar radio frequency device. Dermatol Surg. 2008;34:204–209.
9. Alster TS, Tanzi EL. Cellulite treatment using a novel combination of radiofrequency, infrared light, and mechanical tissue manipulation device. J Cosmet Laser Ther. 2005;7:81–85.
10. Wanitphakdeedecha R, Manuskiatti W. Treatment of cellulite with a bipolar radiofrequency, infrared heat, and pulsatile suction device: a pilot study. J Cosmet Dermatol. 2006;5:284–288.
11. Manuskiatti W, Wachirakaphan C, Lektrakul N, Varothai S. Circumference reduction and cellulite treatment with a TriPollar radiofrequency device: a pilot study. J Eur Acad Dermatol Venereol. 2009;23:820–827.
12. Manuskiatti W, Boonthaweeyuwat E, Varothai S. Treatment of striae distensae with a TriPollar radiofrequency device: a pilot study. J Dermatolog Treat. 2009;20:359–364.
13. Boisnic S, Divaris M, Nelson AA, Gharavi NM, Lask GP. A clinical and biological evaluation of a novel, noninvasive radiofrequency device for the long-term reduction of adipose tissue. Lasers Surg Med. 2014;46:94–103.
14. Nootheti PK, Magpantay A, Yosowitz G, Calderon S, Goldman MP. A single center, randomized, comparative, prospective clinical study to determine the efficacy of the VelaSmooth system versus the Triactive system for the treatment of cellulite. Lasers Surg Med. 2006;38:908–912.
15. Querleux B, Cornillon C, Jolivet O, Bittoun J. Anatomy and physiology of subcutaneous adipose tissue by in vivo magnetic resonance imaging and spectroscopy: relationships with sex and presence of cellulite. Skin Res Technol. 2002;8:118–124.
16. Shapiro SD, Eros Y, Abrahami Y, Leviav A. Evaluation of safety and efficacy of the TriPollar technology for treatment of wrinkles. Lasers Surg Med. 2012;44:453–458.
17. Beilin G. Home-use TriPollar RF device for facial skin tightening: Clinical study results. J Cosmet Laser Ther. 2011; 13:69–76.
18. Coleman SR, Sachdeva K, Egbert BM, Preciado J, Allison J. Clinical efficacy of noninvasive cryolipolysis and its effects on peripheral nerves. Aesthetic Plast Surg. 2009;33:482–488.
19. Kemmler W, Schliffka R, Mayhew JL, von Stengel S. Effects of whole-body elecromyostimulation on resting metabolic rate, body composition, and maximum strength in postmeno-pausal women: the Training and ElectroStimulation Trial. J Strength Cond Res. 2010;24:1880–1887.